Prostatitis comes in two forms - acute and chronic. If acute inflammation is quickly treated with antibiotics, chronic prostatitis becomes a serious problem in older men, which has a negative impact on quality of life. Chronic prostatitis can be caused by infection and congestion in the pelvic organs. The disease requires long-term and complex treatment.
Classification of diseases
Chronic prostatitis in men is divided into two types - congestive (abacterial, congestive) and infectious.
Chronic congestive prostatitis is the result of prostate trophism disorders. The disease develops with heart failure or lack of sex life.
Chronic abacterial prostatitis is characterized by severe symptoms and the absence of acute pain syndrome. When analyzed, no infectious agents were detected in prostate secretions, hence the disease is referred to as bacteria.
Chronic infectious prostatitis is the result of untreated bacterial inflammation. The disease begins with an acute form due to infection of the prostate gland. The disease becomes chronic due to lack of adequate and timely therapy. Chronic infectious prostatitis is characterized by periodic exacerbations.
The cause of chronic non-communicable prostatitis
Speaking of chronic prostatitis, most often we mean non-communicable diseases triggered by congestion in the pelvic organs. This is due to violations of prostate trophism - blood circulation, lymph flow, outflow of prostate secretions.
This form of the disease is directly related to lifestyle and is considered a disease of office workers. The main cause of the development of congestive prostatitis is physical inactivity.
Among the factors that tend to the development of congestive prostatitis, there are:

- inactive work;
- lack of regular sports;
- unbalanced diet;
- obesity;
- bad habits;
- varicose veins;
- hemorrhoids;
- Irregular sex life.
The disease develops against the background of any condition, accompanied by circulatory disorders in the lower limbs. Often, prostatitis appears with obesity, when, as a result of increased pressure on the lumbar region and lower limbs, metabolic processes in this zone are disrupted.
If due to the uniqueness of your profession you have to sit all day, you have to move at least in the evening.
Bad habits can trigger the development of prostatitis. Smoking damages blood vessels and disrupts normal blood flow. Due to the physiological characteristics of a person, this mainly affects the blood circulation in the lower legs and pelvic area.
Sex plays an important role in the function of the prostate gland. The optimal amount of intercourse per week for men over 40 is 3-4. The smaller the amount leads to a violation of the outflow of prostate secretions, the greater the amount causes the thinning of the organs.
Another cause of congestive prostatitis is heart failure. The disease is characterized by impaired blood circulation, including in the pelvic organs.
Causes of the development of chronic infectious prostatitis
Chronic bacterial prostatitis is the result of acute inflammation of the untreated prostate gland. This form of the disease is characterized by severe symptoms and the presence of pathogenic agents present in the prostate secretion.
The most common causative agent of infectious prostatitis:

- E. coli and Pseudomonas aeruginosa;
- staphylococcus and streptococcus;
- klamidia;
- ureaplasma;
- Trichomonas;
- fungal flora.
Infection enters the prostate gland in three ways: through the bloodstream, lymph, or through the urethra. The pathway of final penetration of pathogenic agents occurs in case of infection with chlamydia, ureplasma or Trichomonas.
Causes of the disease:
- decreased immunity;
- severe hypothermia;
- pressure;
- long-term antibiotic therapy.
Conditional pathogenic bacteria are always present in the body, and only strong immunity does not allow them to activate.
Chronic bacterial prostatitis develops from the acute form in the following cases:
- presence of chronic infection focus;
- antibiotic therapy chosen incorrectly;
- late termination of treatment;
- weakened immunity.
In most cases, the chronic form of the disease develops precisely due to improper treatment. This occurs when antibiotic therapy schemes are not properly structured or self-treatment. Stopping antibiotics when you feel better causes the disease agent to be completely eradicated. Any decrease in immunity or hypothermia in this case leads to the recurrence of the disease.
The most difficult to treat is fungal prostatitis caused by a yeast-like fungus. These pathogens rapidly develop resistance to antifungal drugs, which makes treatment difficult and increases the risk of developing chronic forms of the disease.
Symptoms of the disease
In chronic prostatitis, the symptoms are mild, however, with decreased immunity or after stress, the disease worsens.
The most common symptoms of chronic prostatitis in men are:
- urinary disorders;
- weight on prostate;
- potential vulnerabilities;
- urges night to use the toilet.
With the worsening of chronic prostatitis, pain in the bladder and perineum is observed. The frequency of urging to the toilet can reach 10 hours. At the same time, the flow of urine is weak, it is necessary to tense the muscles to urinate, but the process itself does not bring relief, and repeated urges appear after a few minutes.
Symptoms and treatment of chronic prostatitis depend a lot on the form of inflammation. With congestive prostatitis, erectile problems are common. This is due to disrupted blood circulation. Ejaculation can occur quickly, or not at all due to thickening of the prostate thickening.
If there is infectious inflammation in the prostate gland or chronic bacterial prostatitis, pain during urination and burning in the urethra after ejaculation may occur. Such symptoms are accompanied by irritation of the urethral mucosa by disease-causing agents contained in prostate secretions.
Prostatitis and erectile dysfunction

Inflammation of the prostate is invisible to the eye, the symptoms of chronic prostatitis have no visible manifestations, but refer to internal disorders. One of the hallmarks of this disease is a weak erection.
Erectile dysfunction in congestive prostatitis develops in several stages. The disease itself can persist for a long time without severe symptoms, and signs of prostatitis will appear only with a weakened immune system.
Inflammation of the prostate in bacteria can be suspected by erectile changes. At the onset of disease progression, an increase in potential is observed. The man was quickly aroused, but ejaculation also appeared quickly. This is due to changes in the viscosity of the secretion of the prostate gland. Discomfort may be felt during ejaculation, but pain is a characteristic of infectious but not congestive prostatitis.
This causes a number of psychological problems that exacerbate the course of the disease. Erectile dysfunction due to problems with blood flow is exacerbated by the fear of sexual partners, which can lead to the development of impotence against the background of prostatitis.
Urine Disorders
Urodynamic problems are observed in all forms of prostatitis.
Chronic abacterial inflammation is characterized by the urge at night to urinate. It is caused by swelling of the prostate gland, which worsens at night. There is a decrease in urine pressure and the need to tighten the pelvic floor muscles to urinate. At the same time, he feels heavy and full in the bladder, and occasional cramps may appear. Due to frequent urges to use the toilet at night, sleep problems and insomnia arise. All this affects the psychological state of men and worsens the course of the disease, because against the background of stress there is a decrease in immunity and a slowdown of metabolic processes.
Men often complain of cramps in the lower abdomen, which is explained by increased tone of the bladder muscles. Typically, symptoms of severe prostatitis are noted with decreased immunity. Without exacerbating the disease, the pain syndrome may not be completely present.
Congestive prostatitis is characterized by severe prostate edema. The contours of the organs become obscure, the prostate itself swells and enlarges. In this case, there may be a feeling of fullness in the rectum and an increase in discomfort during defecation. Problems with urination are caused by compression of the urethra by a swollen prostate gland.
Why is prostatitis dangerous?

The consequences of chronic prostatitis depend on several factors:
- patient age;
- severity of symptoms;
- current time frame;
- effectiveness of drug therapy.
The longer a man lives with chronic prostatitis, the worse the disease becomes. In most cases, the urinary system is affected. With bacterial prostatitis, a kidney infection may occur during urine flow. This is due to the entry of pathogenic agents into the urethra during ejaculation.
Persistent irritation of the bladder and urethra can cause inflammation. Against the background of prostatitis, cystitis and urethritis of various natures are often diagnosed.
In chronic prostatitis, the consequences affect the man's psycho-emotional state. Potential violations, frequent desire to use the toilet, discomfort in the bladder - all this leads to the development of stress. Prostatitis can be an indirect cause of neurosis and depression.
Nervous system disorders with a background of persistent discomfort in the genitourinary organs cause decreased immunity and deterioration of all metabolic processes in the body. Thus, prostatitis causes nerve disorders, which in turn exacerbate the course of the disease, and the coil is closed.
Persistent discomfort, impaired ability, inability to sleep - all of these greatly affect quality of life.
Disease Diagnostics
If you suspect prostate inflammation, you should see a urologist or andrologist. The following diagnostic methods are used to make the diagnosis:
- prostate rectal palpation;
- Ultrasound and TRUS organs;
- kidney ultrasound;
- prostate secretion analysis;
- PSA blood test.
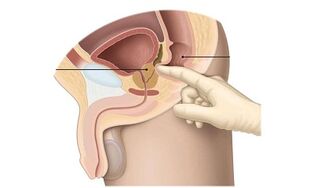
The need for further examination is determined after palpation of the rectal organ. This procedure is also known as prostate massage. The doctor inserted two fingers into the rectal opening and felt the prostate. Inflammation is evidenced by changes in organ structure, tissue heterogeneity and prostate contour. During the massage, the organs are stimulated and prostate secretions are secreted from the urethra. It was collected for further analysis. Prostate secretion analysis shows:
- total lecithin seeds;
- number of leukocytes and erythrocytes;
- presence of pathogenic microorganisms;
- presence of fungal microflora.
This can not only determine the nature of the inflammatory process, but can also identify the causative agent of infectious prostatitis.
Ultrasound and TRUS are performed to remove stones in the prostate rather than diagnosing prostatitis, as the method is less informative, in contrast to secretory analysis.
PSA blood tests are prescribed to exclude oncopathology of the prostate gland. It also detects inflammation or prostate adenoma. How to treat chronic prostatitis depends on the test results and the type of inflammation.
Characteristics of treatment
Chronic prostatitis treatment regimen is a combination of medical, physiotherapy and folk methods. The treatment comes with lifestyle changes - adjusting the menu, letting go of bad habits, normal sports and sex life.
It is important to understand that for chronic prostatitis, treatment will take at least six months. In addition to drugs to relieve inflammation, men are given long-term rehabilitation therapy, which is needed to normalize the function of the prostate gland.
Medicine
How to cure chronic prostatitis depends on the form of the disease. Remedies for chronic prostatitis include:
- antibiotics or anti-inflammatory drugs;
- rectal suppositories to normalize trophism;
- immunostimulants and general health improvement agents.
For the treatment of chronic prostatitis in men, antibiotics are used, but only if it is an infectious prostate inflammation. How to treat infectious prostatitis in men depends on the pathogen and the success of the previous course of therapy. In acute bacterial inflammation, macrolide antibiotics are prescribed in most cases. They effectively suppress the activity of pathogenic agents and are distinguished by a broad spectrum of action. In the absence of adherence to the wrong treatment regimen or medication, the microorganisms that cause inflammation rapidly develop resistance to macrolides, which largely determine the transition of the disease to a chronic form.
Fluoroquinolones is an effective antibacterial agent for microbial prostatitis. They have a clear anti-inflammatory activity against various pathogenic microorganisms.
Although fluoroquinolones do not have natural analogues, which is the reason for the lack of resistance of pathogenic microorganisms to the action of the drug, it is necessary to carefully follow the treatment regimen chosen by the doctor. Otherwise, the drug is ineffective and antibiotic therapy should be repeated.

Antibacterial drugs and tablets are not used to treat non-communicable chronic prostatitis. With congestive prostatitis, inflammation is caused not by microbes, but by violations of trophism, therefore, it is inappropriate to use antibiotics for treatment. They use anti-inflammatory drugs. They are used in short courses to reduce inflammation and swelling. This medicine is prescribed in suppositories or injections. Treatment requires an average of one week, the drug is given rectally at night or intramuscularly once a day. If there is severe inflammation, it is possible to use the drug twice during the day.
Anti-inflammatory drugs are not antibiotics. Tablets are successfully used to relieve the inflammatory process with non-infectious or congestive prostatitis. On average, doctors prescribe two tablets daily for 5 days, and then transfer the patient to therapy with phytopreparation that enhances prostate trophism.
If there is a severe urinary incontinence, treatment is complemented with drugs of the alpha-blocker group. These drugs loosen the bladder, reducing muscle tone, thus allowing urine to flow normally. Drugs in this group are taken one tablet a day in short courses, treatment with alpha blockers rarely lasts more than a week.
Once the inflammation has stopped, congestive (cognitive) and infectious prostatitis is treated with drugs that normalize prostate gland trophism. Drugs contribute to:
- reduces inflammation;
- pain relief;
- normalization of urine;
- potential increase.
For chronic prostatitis, this medication is used for at least two weeks. They come in the form of rectal suppositories. The recommended dose is one candle daily at night.
Propolis suppositories are recommended to restore local immunity. They relieve inflammation, increase blood circulation and the outflow of prostate secretions, and also significantly increase immunity, preventing the deterioration of prostatitis. The drug comes in the form of small suppositories that are injected into the rectum at night.
In addition, your doctor may recommend suppositories with ichthyol. They relieve inflammation and reduce swelling of the prostate gland.
Preparations based on echinacea extract are recommended as a general tonic for prostatitis. They strengthen the immune system and prevent the development of prostatitis. With the onset of neurosis and insomnia against the background of prostatitis, doctors may recommend sedatives.
Physiotherapy for chronic prostatitis
The cause of chronic prostatitis lies in poor blood circulation in the pelvic organs. To speed up the recovery and recovery of prostate trophism, physiotherapy methods are widely used:
- magnetic therapy;
- electrophoresis;
- shock wave therapy;
- acupuncture.
Acupuncture (acupuncture) and leech therapy (hirudotherapy) are distinguished from non-traditional methods.
There are many home physiotherapy methods. The most popular are special devices. They create alternating magnetic fields that have a positive effect on metabolic processes, relieving congestion in the pelvic organs.
Darsonvalization can also be used at home. These are micro-effects that enhance metabolic processes. You can buy tools for treatment at home at any medical equipment store, but it is recommended that you see a doctor first.
Prostate massage is used to treat congestive prostatitis. It is performed by specialists in medical facilities. Organ stimulation allows you to eliminate edema and discomfort, as well as relieve blocked prostate secretions. The course of treatment consists of 10-15 procedures.
People's solution
Whether chronic prostatitis is treated depends on the various therapeutic steps taken. Traditional medicine will help complete drug treatment.

Homemade suppositories are used to relieve inflammation in the prostate. To prepare the wax, you need 200 g of base fat, 40 ml of propolis extract. The base is diluted in a water bath, propolis is slowly poured into it, stirring constantly. When the product acquires a uniform color, the product is poured into a layer of adhesive and packaged in the form of sausage. The mass should be cooled for an hour until cool. When the product has cooled, it is divided with a knife into the same torpedo-shaped pieces, about 5 cm long and 2 cm in diameter. These candles should be stored individually packaged in the refrigerator. The recommended dose is a suppository to the opening of the rectum before bedtime. The duration of treatment is 2-3 weeks.
You can also make candles with honey and honey seed oil. The proportions are 200 g of base, 50 ml of oil and 3 tablespoons of honey. As a base, you can take beeswax, lanolin, cocoa butter. Such suppositories relieve inflammation, improve prostate function and enhance immunity.
To cure chronic prostatitis at home, you can use various infusions and decoctions. One of the most effective remedies is parsley juice. It must be taken 3 tablespoons daily.
Traditional medicine recommends eating 30 g of pumpkin seeds per day. They contain many nutrients needed for the normal functioning of the prostate gland.
Another effective treatment is a mixture of pumpkin seeds, walnuts, and honey. To prepare the medicine, you should take 100 peeled seeds and the same amount of walnuts, place in a suitable container and pour 500 ml of honey. The product is stored in the refrigerator for 4 days to put, and then 4 tbsp is taken daily.
Surgical Treatment
Whether chronic prostatitis can be cured permanently depends on the severity of the disease and the age of the patient. With frequent swelling, you should always take medication.
Surgical treatment of prostatitis in most cases is not performed. Probably the use of radical measures - complete removal of the prostate gland. Such surgery is performed only if the prostate does not fulfill its function due to chronic inflammation, and drug treatment is ineffective. In addition, prostate removal is performed at risk of oncology.
Interestingly, the effects of prostatitis are usually observed in old age, in men over 65 years of age. In this case, a number of difficulties arise in treatment:
- diseases of the cardiovascular system;
- contraindications to taking medication;
- many side effects.
Many men, who have been suffering from prostatitis for more than 10 years, insist on undergoing surgery. This is usually associated with poor drug tolerance and a large number of side effects. Doctors say that surgery is the last resort, and with the right approach, prostatitis can be cured by conservative methods.
Prevention and prognosis
After learning what chronic prostatitis is in men and how dangerous it is, the question arises as to whether the disease can be completely cured.
Patient testimonials show that chronic prostatitis can be cured, but will take a long time. The duration of treatment requires an average of six months or more. Urologists agree that adequate therapy, lifestyle changes and a balanced diet will help eliminate inflammation.
Often, swelling and inflammatory episodes recur after prolonged remission are faced by men who do not follow the doctor's recommendations, but are treated on the advice of friends. It is important to understand that success in therapeutic treatment depends on the selection of the right drug therapy. Leading to exacerbation or re-manifestation of the symptoms of chronic prostatitis can be:
- unsystematic medication intake;
- non-compliance with doctor's recommendations;
- discontinue treatment after the first improvement;
- bad habits;
- lack of physical activity.
Self-medication often causes deterioration in well-being. This is especially true in cases of infectious inflammation, when patients choose antibiotics independently without testing.
The most common mistake men make is stopping treatment when the first improvement appears. In this case, the inflammation does not disappear, but only diminishes briefly. With a decrease in immunity or hypothermia, the disease will be felt again.
In addition to medication, prostatitis requires lifestyle changes. It is important to abandon bad habits, normalize nutrition and start playing sports. With prostatitis, it is recommended to do yoga, exercise therapy, swimming. Any exercise involving the pelvis will be beneficial. Men with this condition, especially inactive, should exercise for 10 minutes daily and do full exercise several times a week. Also, during the treatment of chronic prostatitis, it is necessary to have sex, as regular ejaculation helps reduce prostate edema.
The success of prostatitis treatment depends on a timely diagnosis, therefore, if you notice problems with urination, you should see a urologist as soon as possible.






























